July 28 is World Hepatitis Day.
According to the World Health Organisation, 10 – 15 per cent of Vietnam’s population is estimated to have viral hepatitis, including 1,07 million people who have Hepatitis C. Over 90 per cent of those who have Hepatitis C are not aware of their positive status.
OUCRU, the Hospital for Tropical Diseases (Ho Chi Minh City), and Vietnam’s National Hospital for Tropical Diseases (Hanoi) have been collaborating on Hepatitis C clinical trials since 2018. Our research is centred around predictive factors for selecting persons who could be successfully treated with shorter durations of antiviral therapy for Hepatitis C.
Currently, directly acting antiviral (DAA) therapy for Hepatitis C (HCV) offers high cure rates to those able to adhere to standard durations of treatment. In low- and middle-income countries like Vietnam, where treatment is limited to second-generation NS5A/NS5B-inhibitor combinations, the standard treatment is at least 12 weeks. This duration presents a barrier to successful engagement in care for some populations, hampering the elimination of HCV as a public health threat. Novel treatment strategies are required for hard-to-reach individuals, such as people who inject drugs and those with no fixed abode.
In addition, in Vietnam, DAA therapy for Hepatitis C remains prohibitively expensive for many of those infected. A standard twelve-week course of sofosbuvir and daclatasvir (SOF/DCV) was priced at US$2,417 – $2,472 in Ho Chi Minh City in 2019. Despite the government subsidising 50% of drug costs since, the Ministry of Health estimates only 1,000 individuals accessed DAA treatment through health insurance in 2019 and 2,700 in 2020.
The World Health Organisation has called for research into predictive factors for selecting persons who could be successfully treated with shorter durations of therapy, which could expand access to treatment and reduce drug costs.
We completed a small pilot study in 2020, looking at the early virological response as a means of guiding the duration of therapy of SOF/DCV, which remains the lowest-priced and most widely available treatment option globally.
We are also running an ongoing larger multi-arm randomised controlled trial exploring three different treatment shortening strategies for Hep C with two different drug combinations. We expect to complete recruitment in early 2023.
In addition, our team of OUCRU researchers recently performed a systematic review and meta-analysis of the seroprevalence of Hepatitis B, C and D in Vietnam from 1990-2020, which was published in The Lancet Western Pacific in May 2022. We found that while blood safety has improved, a renewed focus on HBV vaccination at birth and targeted HCV screening and treatment of people who inject drugs are urgently required to meet elimination targets.
To date, these clinical trials have recruited from populations already engaged in care at the HTD. Participants are aware of HCV infection and its implications and are well-motivated to seek treatment. Since our clinical trials are investigating the efficacy of treatment strategies that could be used to treat underserved populations (e.g. ultrashort or intermittent therapy), should these strategies have efficacy as hoped, it is crucial to develop innovative ways to engage with these ‘hard-to-reach’ populations, such as people who inject drugs (PWID), men who have sex with men, commercial sex workers, as well as low-income communities.
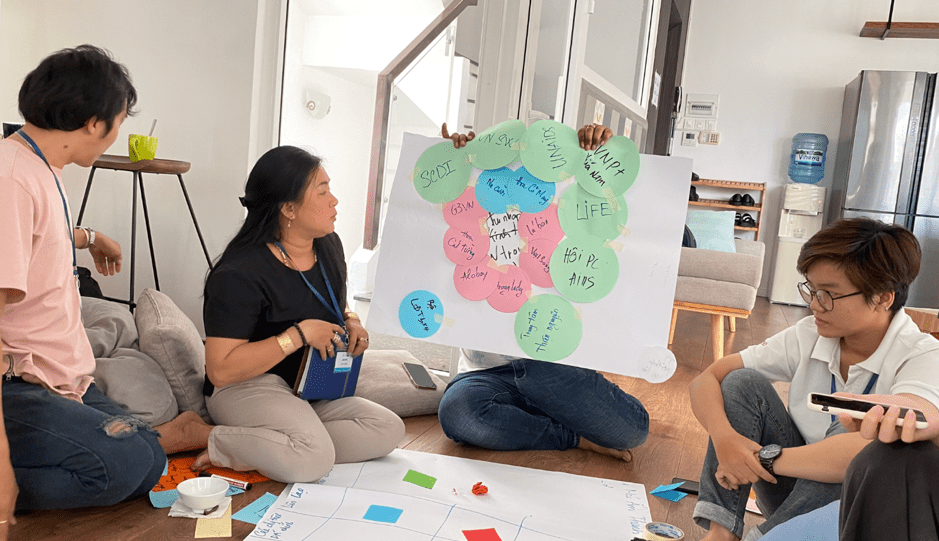
OUCRU’s social science and public engagement teams are currently working with these underrepresented groups, using community-based participatory research (CBPR) to engage with communities to create community-led strategies to improve linkages to care and treatment for populations at risk for viral hepatitis.
These studies are currently ongoing, with a positive impact on the participants. We hope to have a more significant impact on the treatment strategy and access to care for patients with Hepatitis C in Vietnam and worldwide in the future.





