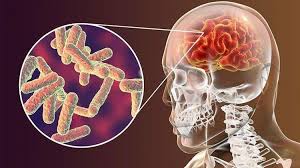
Tuberculous meningitis (TBM) is a form of tuberculosis that carries the highest mortality rate due to its gradual onset, non-specific symptoms, and easy confusion with other brain infections.
The World Health Organization (WHO) estimates that children account for 10-12% of new and recurring TB cases annually. Approximately 70,000 infants and children die from TB each year(1).
TBM represents 1-5% of total TB cases. While it can occur at any age, in children, TBM most commonly affects the age group 1 to 5, a time when their brains are still immature. Insults or infections of the brain at this time can have long lasting affects, such as disability.
In 2022, WHO made a conditional recommendation that a shorter 6-month intensive TB drug regimen with aspirin could be used an alternative to the standard 12-month treatment, based on a systematic review and meta-analysis of observational studies showing reduced mortality in children with TBM. This shortened regimen would potentially have large benefits for families and health systems.
In partnership with our international partners including Medical Research Council, University College London, Wellcome Trust, UKAID, and National Institute for Health and Care Research, OUCRU conducts a randomised controlled trial to evaluate whether this 6-month regimen is as effective and safe as the standard 12-month treatment for children with TBM between 29 days and 18 years of age.
“I have come back to life after I recovered from meningitis TB for more than 13 years ago. With only 2% chance of survival in the emergency room and I was in a coma for nearly half a year, I got 18 months of treatment due to drug resistance and I also spent many years after that to receive rehabilitation treatment and return to life. Although I have the sequelae that make me a person with a particularly severe disability, I am proud that I have done the job which is social work that I dreamed of since childhood, and I am currently a law student at Open University in Hanoi. I want to send the message to TB patients that: TB meningitis can be completely cured and TB drugs will not destroy the intelligence of who being treated, to recover and return to life effectively, it is necessary to detect the disease early and comply with the correct treatment to minimize the sequelae”.
Working closely with TBM-affected children and their families revealed their unique challenge to the project team. This community’s needs overlap between multiple areas—clinical care, research, and policy programme—often resulting in gaps in comprehensive care. Using the World Health Organization (WHO) “Defeating Meningitis by 2030: global roadmap” as a framework, the SURE project team at OUCRU explored ways to better support children with TBM across five key areas: diagnosis and treatment, surveillance, support and care for affected people, and advocacy and engagement.
Through this TBM research project, Dr Julie Huynh and the project team at OUCRU discovered that caregivers of children who are affected by TBM face several challenges including a lack of post-hospital discharge support systems and the financial, medical, and emotional burden of caring for their child who leaves hospital with disability.
“As a paediatrician, it is gut-wrenching to see young, previously healthy children die from TB meningitis, or live with some form of disability if they are fortunate to survive. The first thing parents ask me when the diagnosis is given is ” Will my child be ok? Will his/her brain be normal? Will they be able to go to school and do the normal things children do?”. This is what our research at OUCRU is about. It’s about improving the lives of children who are affected by this devastating illness and their families who care for them”
To address these challenges, Dr Julie Huynh collaborated with the Public and Community Engagement group to establish a community advisory board (CAB) consisting of 5 family members (parents/carers) of children who have survived TBM but with long lasting effects. The project team plans to gather insightful feedback from the board members, develop and pilot several support packages for TBM survivors’ families.
Given that most hospitalised cases are severe, difficult to diagnose, and often result in serious long-term consequences even after successful treatment, this community-based approach is particularly important in helping to lighten the burden on TBM survivors’ families and address the gap in institutional support.
A booklet of care instructions and rehabilitation guidelines
Beyond providing valuable insights, board community members collaborate with Dr Julie and the project team to co-design a visual booklet containing guidelines and care instructions for parents of children living with disability at home. The resource will receive technical oversight from Dr Julie and incorporate special contributions from a TBM survivor, combining professional expertise with practical, real-life experience.