Vietnam remains a country with a high tuberculosis burden, with tuberculous meningitis (TBM) being particularly challenging to detect early, often leading to severe neurological sequelae in patients.
TBM has a mortality rate of 20%–50%, and neuro-disability occurs in up to 50% of survivors(1). One of the biggest challenges in diagnosing TBM is that its clinical symptoms are quite similar to other brain infections.
Despite its dangers, TBM can be prevented with the BCG vaccine (Bacille Calmette-Guérin). However, many parents have admitted that their children either haven’t been vaccinated at all or don’t have up-to-date vaccinations.
With the mission of addressing global health issues, Collab Lab, an initiative led by OUCRU’s Public and Community Engagement group, has chosen to animate a publication about TBM, aims to raise awareness about tuberculosis in general, TBM, and the importance of BCG vaccination for children.
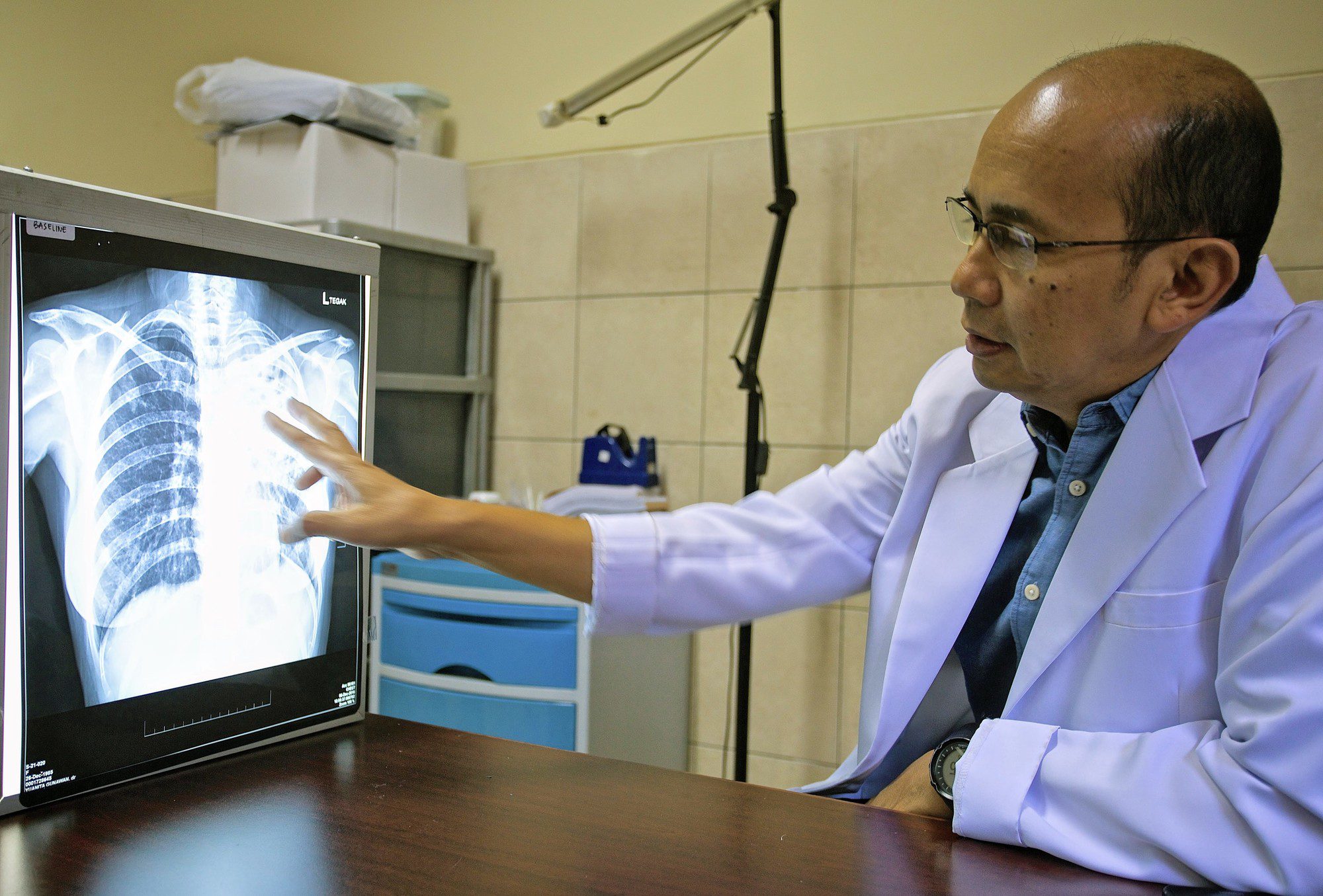
“I thought TB only affects the lungs”.
According to the World Health Organization’s (WHO) 2020 report, Vietnam ranks 11th among 30 countries with the highest number of tuberculosis cases and 1st in terms of multidrug-resistant tuberculosis burden globally(2). Annually, Vietnam records over 172,000 tuberculosis cases and 10,400 deaths due to the disease. In Ho Chi Minh City alone, the first six months of 2022 saw more than 8,434 tuberculosis cases, an increase of over 33% compared to the same period in 2021(3).
Tuberculous Meningitis is a severe form of tuberculosis that affects the membranes covering the brain and spinal cord. Dr. Truong Huu Khanh, Vice President of the Ho Chi Minh City Infectious Diseases Association, states that tuberculous meningitis has the highest mortality rate among tuberculosis-related diseases in newborns, with a mortality rate of 20-50%(4).
More than 50% of survivors have severe neurological sequelae such as cerebral palsy, limb paralysis, epilepsy, muteness, deafness, or blindness. Patients may also develop other long-term complications like dementia, nerve damage, and mental disorders.
One of the biggest challenges in diagnosing TBM is that its clinical symptoms are quite similar to other brain infections. Therefore, early diagnosis before brain damage occurs is the most important prognostic factor for survival and the extent of sequelae impact on patients.
Diagnosing TBM using genes
Recent reports have shed new light on diagnosing TBM. They’ve discovered that certain genes—GPB5, DUSP3, and KLF2—show significant expression changes in patients with pulmonary tuberculosis. The question now is whether these genetic markers are reliable enough to be applied in the early diagnosis of tuberculous meningitis.
A recent publication by Dr Julie Huynh, Clinical Research Paediatrician at OUCRU, aims to develop a simple and effective test for TBM. This test could distinguish TBM from other brain infections, thereby enhance the speed and accuracy of diagnosing TBM, improve treatment quality and reduce sequelae for patients with TBM.
Raising awareness of TB vaccines is essential to improve vaccine uptake
Other than the challenges in diagnosis, the awareness of the importance of TB vaccines among parents is another factor affecting children’s TBM infection rates. Several families with TBM child patients admitted that their children had not received the BCG vaccine or couldn’t remember if their children had been vaccinated at all.
By animating Dr Julie Huynh’s TBM project, Collab Lab seeks to explain TBM’s danger to the human brain, emphasise the significance of early accurate diagnosis, and marking this new milestone in the fight against TB in general and TBM in particular.
Collab Lab’s animated explainer videos aim to make complex genetic research information more accessible to a wider audience, particularly young people, who may play a decisive role in increasing TB vaccine uptake in Vietnamese society.
Reference:
1. Huynh J, Nhat LHT, Bao NLH, Hai HT, Thu DDA, Tram TTB, Dung VTM, Vinh DD, Ngoc NM, Donovan J, Phu NH, Van Thanh D, Thu NTA, Bang ND, Ha DTM, Nghia HDT, Van Tan L, Van LH, Thwaites G, Thuong NTT. The Ability of a 3-Gene Host Signature in Blood to Distinguish Tuberculous Meningitis From Other Brain Infections. J Infect Dis. 2024 Aug 16;230(2):e268-e278. doi: 10.1093/infdis/jiad606. PMID: 38169323; PMCID: PMC11326836.
2. https://vnexpress.net/who-canh-bao-so-ca-benh-lao-tang-cao-ky-luc-4810615.html
3, 4. https://vnexpress.net/nhieu-em-be-mac-lao-mang-nao-nhap-vien-4546696.html