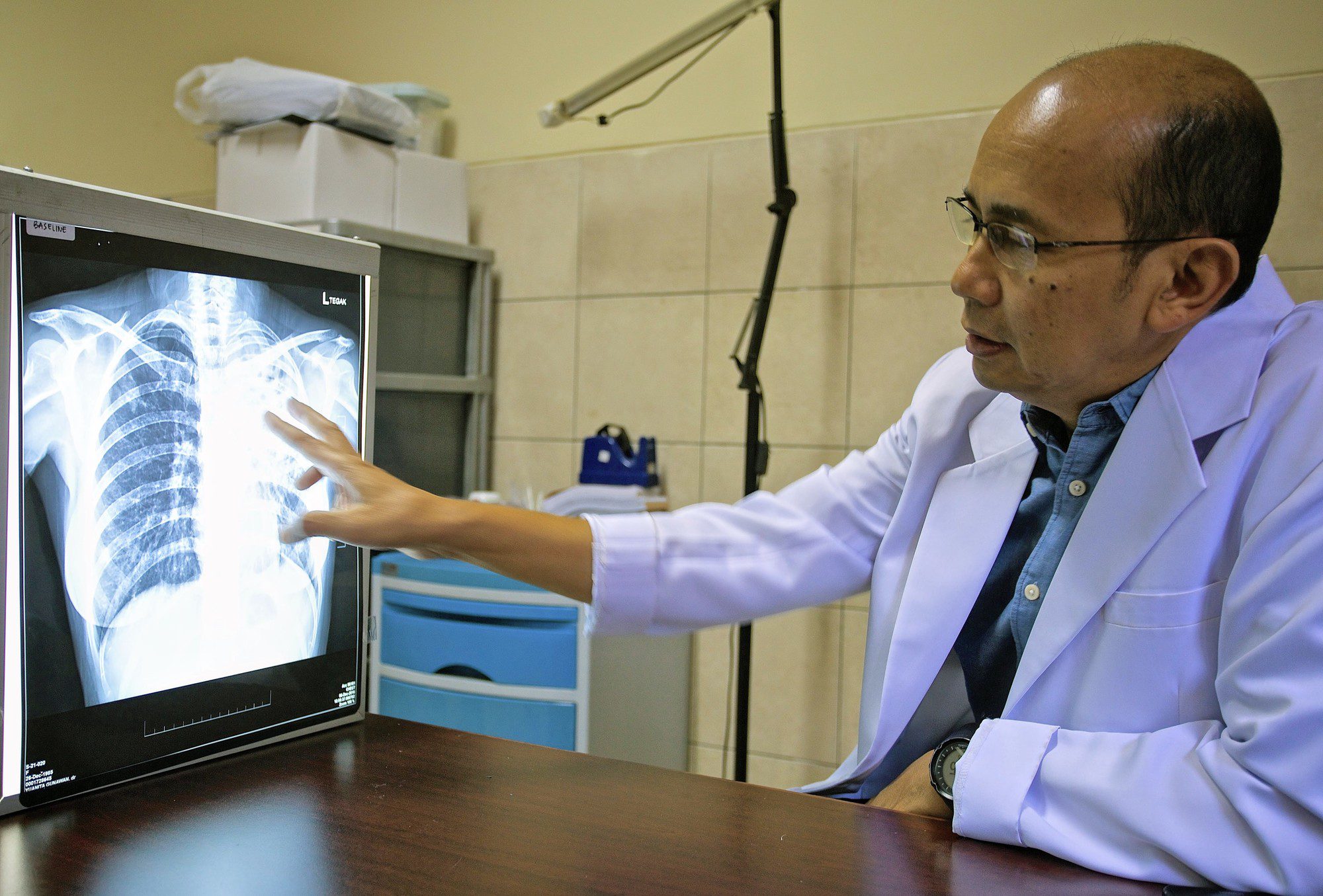
Tuberculous meningitis is a dangerous condition caused by the bacteria responsible for tuberculosis spreading from the lungs to the brain. It affects more than 150,000 adults a year worldwide, and results in death or brain damage in half of all patients. People living with HIV are particularly at risk for negative outcomes.
These severe forms of tuberculous meningitis may be linked to the immune system becoming over-active while trying to fight the disease and harming the brain in the process. Detecting this hyperinflammation via blood sample analyzes has remained challenging so far, as traditional approaches can only offer partial information on the inflammatory response.
In a new paper published in eLife, OUCRU researchers took advantage of new genetic approaches to examine the expression of around 20,000 genes in the blood of HIV-positive and HIV-negative patients with tuberculous meningitis or lung tuberculosis, as well as in healthy individuals. Identifying which genes are more or less expressed in the different groups of volunteers can help to better understand the mechanisms associated with tuberculous meningitis, particularly in its most dangerous forms. Such analysis could also allow scientists to pinpoint which genes to monitor to efficiently detect patients at higher risk of severe complications.
The results show that tuberculous meningitis mortality was associated with a distinct pattern of immune cell response; white blood cells known as neutrophils were increasingly activated while T and B cells showed decreased activity. Increased mortality was also linked to different patterns of gene activity between patients living with or without HIV. Overall, inflammatory genes were more activated in HIV-positive tuberculous meningitis patients than in their HIV-negative counterparts. Finally, the authors found that the blood activity levels of just four specific genes formed a signature associated with increased risk of death from tuberculous meningitis.
“In the future, medical professionals may be able to use this signature to rapidly identify patients who require intensive care and more specialized treatments,” said Associate Professor Nguyen Thuy Thuong Thuong, who leads the TB research group at OUCRU. “The findings also reveal immune system processes and molecules that may serve as potential drug targets for future therapies against this disease.”
To learn more, visit the published article.
This article was originally published in English on eLife Digest and has been modified for OUCRU’s audiences.