The study, titled “Burden of Bacterial Antimicrobial Resistance in Low-Income and Middle-Income Countries Avertible by Existing Interventions,” provides valuable insights into existing public health interventions that can save lives and curb this global crisis.
Antimicrobial resistance (AMR) occurs when bacteria become resistant to the drugs used to treat them. It is estimated that approximately 5 million deaths annually are associated with bacterial infections resistant to antibiotics. The majority of these deaths, around 4.3 million, occur in low-income and middle-income countries (LMICs), where healthcare systems often struggle to cope.
The research team, including Assoc Prof Abhilasha Karkey from OUCRU Nepal, conducted a comprehensive analysis of existing interventions and their impact on reducing AMR-associated deaths in LMIC settings. Their findings indicate that countries should prioritise certain public health interventions that offer the greatest potential to mitigate the AMR burden.
Using a robust methodology, the researchers examined data from diverse sources, including epidemiological studies, multicountry survey data, and existing meta-analyses. They developed a modelling analysis to estimate the impact of various interventions on reducing AMR-associated deaths in LMICs.
The study highlights three key interventions that have the potential to prevent 750,000 deaths linked to AMR each year:
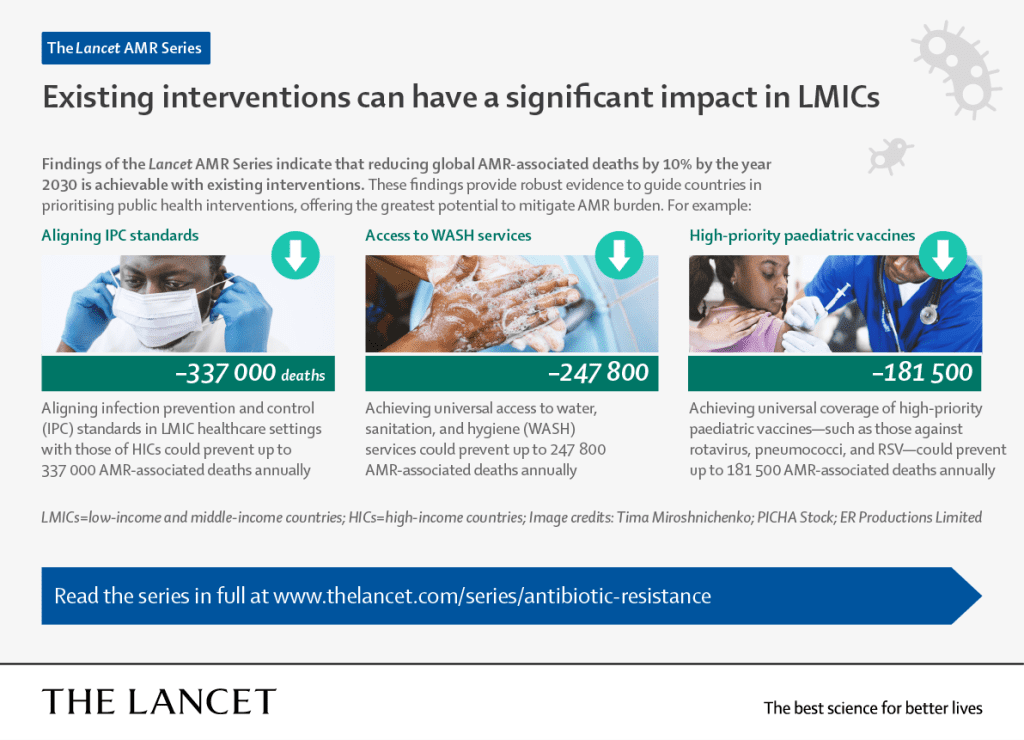
1. Improving infection prevention and control (IPC) programs: Enhancing IPC programs in LMIC healthcare settings could prevent at least 337,000 annual AMR-associated deaths. Despite constraints on WASH infrastructure, effective measures to ensure hand hygiene and proper sanitation (e.g., alcohol-based hand sanitisers, disinfectants and personal protective equipment) can prevent transmission within healthcare facilities and save lives.
2. Ensuring universal access to water, sanitation, and hygiene (WASH) services: Providing high-quality WASH services could prevent up to 247,800 AMR-associated deaths annually. However, it would require heavy investment in physical infrastructure rather than relying on prevailing low-cost measures that focus on individual behaviour changes.
3. Achieving universal coverage of high-priority pediatric vaccines: Access to vaccines could prevent 181,500 AMR-associated deaths annually in LMICs. Vaccines not only protect against resistant infections but also reduce antibiotic consumption.

“Preventive measures are not only critical for saving lives but also for safeguarding the efficacy of existing antibiotics. By prioritising these interventions, we can significantly reduce the global burden of AMR and ensure a healthier future for all.”
Assoc Prof Abhilasha Karkey, Director of OUCRU Nepal
Implementing these interventions is estimated to reduce 18% of AMR-associated deaths occurring in LMICs annually. However, it is crucial to note that these interventions are not mutually exclusive, thus a combination of different methods is necessary to have the best results.
The study underscores the importance of evidence-based policymaking and the need for governments to allocate resources to implement these interventions. It also highlights the role of international collaboration in sharing knowledge, resources, and best practices to combat antibiotic resistance globally.
Read the series on The Lancet.






