Addressing the global health crisis
Antimicrobial resistance (AMR) is a growing global health emergency that threatens to reverse decades of medical progress. In Vietnam, the issue is particularly acute in underserved regions, where healthcare resources are often limited and diagnostic tools are scarce.
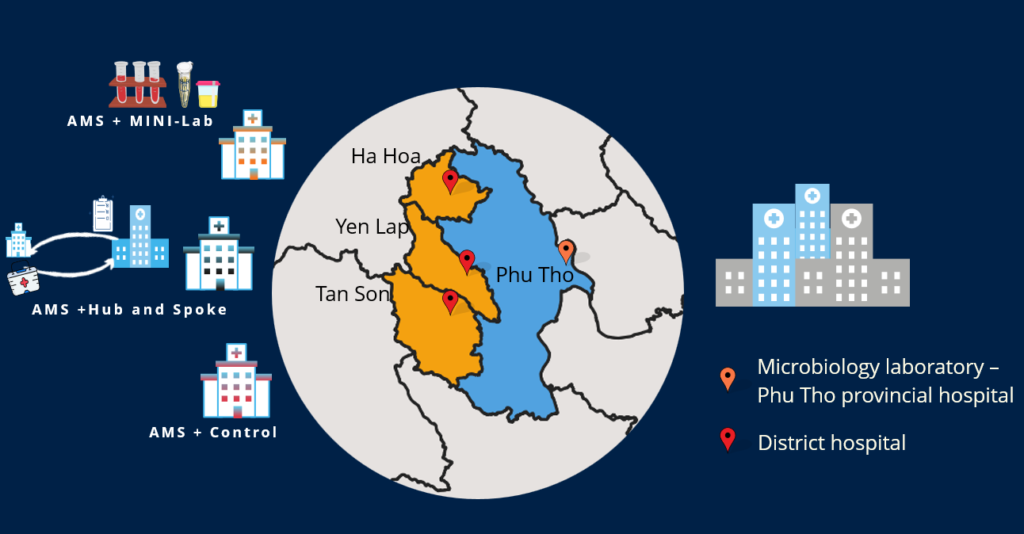
In Phu Tho, a province in northern Vietnam, districts like Ha Hoa, Yen Lap, and Tan Son are particularly vulnerable due to the lack of microbiological facilities. This absence of essential laboratories forces patients to travel to provincial hospitals for testing, a barrier that delays diagnosis and treatment.
Without proper diagnostic tools, doctors frequently prescribe antibiotics based solely on symptoms and clinical judgment. This practice inadvertently contributes to the rise of antibiotic resistance at the district level.

To address this issue, OUCRU and the Phu Tho Department of Health have partnered to strengthen antibiotic stewardship in these resource-limited areas. Specifically, the initiative focuses on upgrading diagnostic capabilities and microbiology laboratory solutions in district-level hospitals.
On November 19, 2024, a semi-final meeting was held to celebrate the project’s positive impact on patient care, antibiotic resistance control, and healthcare practices. Attendees included Dr Nguyen Thanh Ha, Deputy Director of the National Hospital of Tropical Diseases, and representatives from Phu Tho’s Department of Health and provincial hospitals.
Improved patient care through data-driven decisions
Since 2022, the project introduced two microbiology solutions tailored to the specific needs of each study site. In Ha Hoa district, a Mini-lab was set up, offering ready-to-use diagnostic testing for sterile samples (e.g., blood, urine, sterile fluids) directly at the district level.
In Yen Lap and Tan Son districts, a Hub-and-Spoke model was implemented, allowing samples to be sent to a centralised, higher-level laboratory at the provincial hospital for testing.

These solutions offer healthcare providers precise data on bacterial identification and antibiotic susceptibility, enabling more targeted treatment decisions. As a result, doctors can select antibiotics that are specifically effective against the bacteria causing the infection, leading to improved patient care.
This data-driven approach reduces reliance on broad-spectrum antibiotics, minimising the risk of fostering antibiotic-resistant bacteria. Ultimately, it favours the de-escalation of therapy when appropriate and reduces unnecessary antibiotic overuse.
“The availability of microbiology testing at my hospital has changed my approach to treatment. Ordering microbiology tests immediately upon admission has now become a routine practice.”
Dr Tran Thu Hoai, local physician.
Building capacity through training
Beyond technological upgrades, the project equipped healthcare professionals with essential training in critical areas such as antimicrobial stewardship, clinical microbiology, ethical research conduct, and infection prevention and control.
The focus on building local capacity ensures that healthcare providers are not only supported with the necessary tools but also equipped with the knowledge to improve antibiotic use and infection control in their daily practices.
By offering hands-on training, the project has empowered healthcare professionals to make informed, evidence-based decisions that improve patient outcomes and help slow the spread of AMR.
“Thanks to the training programmes of the UMAMIS study, surgeons have changed their perspectives and are now cooperating to implement guidelines for antibiotic prophylaxis in clean surgeries at district health centres,” said clinical pharmacist Nguyen Thi Quynh Huong.
A sustainable model for the future
Following the conclusion of the project, the district health centres in Ha Hoa, Yen Lap, and Tan Son are committed to maintaining the improvements achieved through this initiative.
Studies are in place to ensure the ongoing operation of the Mini-lab, integrate microbiology testing into routine clinical pathways, and expand the range of microbiological tests available at the district level.
“This project has proven that, in resource-limited settings, it is not only possible to implement microbiology testing, but that it supports the antimicrobial stewardship programme and vice-versa.”
Dr Thomas Kesteman, Principal Investigator.

“Preliminary results showed a reduction in antibiotic use, both hospital-wide and in the surgical department,” added Dr Vu Thi Lan Huong, Principal Investigator. “These results have the potential to inform policymakers and funders about the implementation model combining AMS with microbiological interventions. Further analyses are being conducted to assess the impact in more detail.”
“Looking ahead,” commented Dr Luong Duy Dong, Vice Director of Ha Hoa District Health Center, “we hope to maintain the microbiology laboratory at the centre and research collaborations with OUCRU.”
The ongoing commitment to training and collaboration is crucial for sustaining these improvements and creating a self-sustaining cycle of knowledge transfer and improved healthcare outcomes.
***
About the project
The project “Upgrading and Amplifying Antimicrobial Resistance Control with Microbiology Laboratory Solutions for District Hospitals in Phu Tho, Vietnam” is part of a larger initiative, “Extending Antimicrobial Stewardship Programmes to Underserved Clinical Activities: Outpatient Departments and Hospitals Without Bacteriology Capacity in Vietnam.”
This ambitious initiative seeks to expand the reach of antimicrobial stewardship programs and enhance AMR control in underserved areas of Vietnam, particularly in outpatient clinics and district hospitals that lack the infrastructure for microbiological testing.
Dr Thomas Kesteman is the Project Lead cum Principal Investigator and Dr Vu Thi Lan Huong is the Co-investigator.
Funded by Pfizer Global Medical Grants and Global Bridges at Mayo Clinic, and running from January 2022 to September 2024, the project is being implemented in collaboration with the National Hospital of Tropical Diseases, two provincial hospitals (Vietnam – Sweden – Uong Bi Hospital and Dong Thap Provincial Hospital), and three district hospitals in Phu Tho (Ha Hoa, Tan Son, and Yen Lap).